NUTRITIONAL SURVEILLANCE
Pre-Operatively Nutritional Management for Bariatric Patients
Morbid obesity can be enfolded with many other non-communicable diseases and poor quality of life. To get the best possible results after bariatric surgery, it is important to optimize patients preoperatively.

Pre-Operative Nutritional Management :
5-10% of weight reduction pre-op bariatric surgery has a beneficial impact on overall health including physical, clinical and mental health.
Weight reduction through lifestyle management requires dedication, continuous effort and a lot of patience to see expected results. Everyone’s body responds differently to weight loss program. It is always better to compare your results with the amount of effort you put in instead comparing yourself with others.
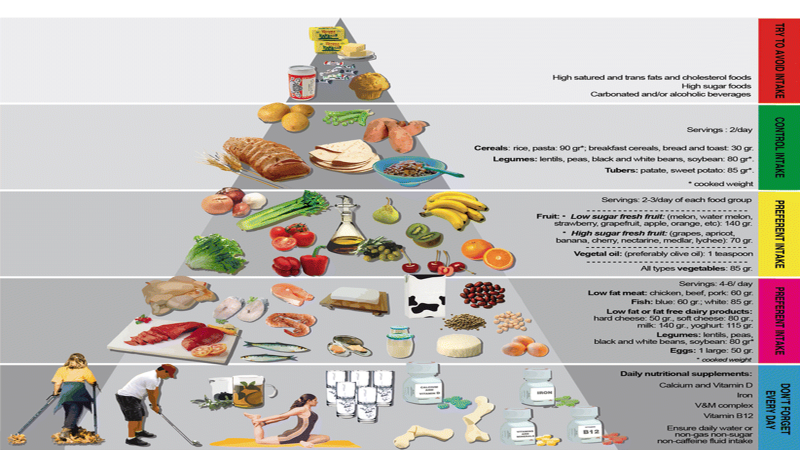
We provide nutritional guidance with emphasis on lifestyle modification on the very first visit to Bariatric surgery OPD/Clinic. We expect a minimum of 2-3 kg weight reduction on the low – calorie diet. This diet is generally a normal diet with portion control. Our emphasis is always on eating a balanced meal in time and balancing it with daily physical activity.
1) Follow your specific diet plan 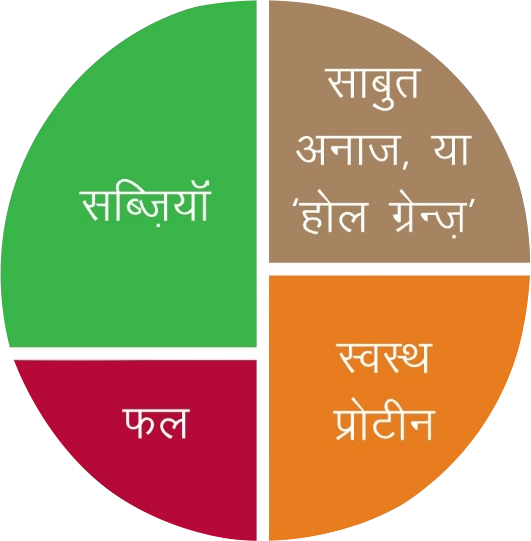
2) Maintain a diet diary. You are on 24 hrs surveillance now.
……A tool to keep an eye on your health investment…….
3) Be regular with physical activity – Exercise with right techniques it acts as fuel for vital organs, save it.



4) We will put you on a very low-calorie liquid diet 15 days(2weeks) prior to surgery-
What we are aiming for…?
This diet will promote moderate ketosis which aids fat loss without losing fat — -free mass, enhance satiety perception, reduces liver volume which provides
greater surgical access and reduces peri-operative complications. There is a general perception that liquid diet can cause constipation and require laxatives for the relief. We have not received any major complaint in this regard from patients who follow VLCD for two weeks. Possible reasons would be the initiation or inclusion of some degree of physical activity, drinking a large volume of fruits and vegetable juices with its pulp and a good amount of fluid intake.
DIET PATTERN
- Skim milk, buttermilk, low-fat yoghurt
- Non sweetened fruit and vegetable juices with pulp, soups, coconut water, lemon water
- Meal Replacer, Optifast VLCD/Obesigo/Getrim/ Essential BLCD ✓ Plenty of plain water
- Tea, coffee without sugar
Assess your compliance on VLCD diet: You can assess your compliance by simple urine investigation
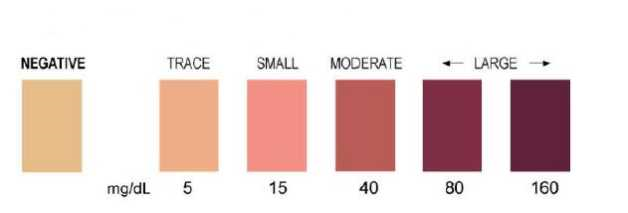
5) Your honest approach can reward you with 3-5 kg weight loss within 15 days.
6) Keep gathering authentic knowledge related to the procedure you are going to opt for your weight loss program.
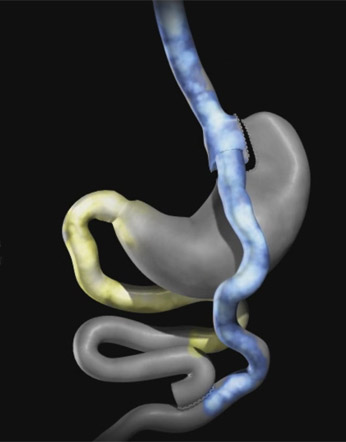
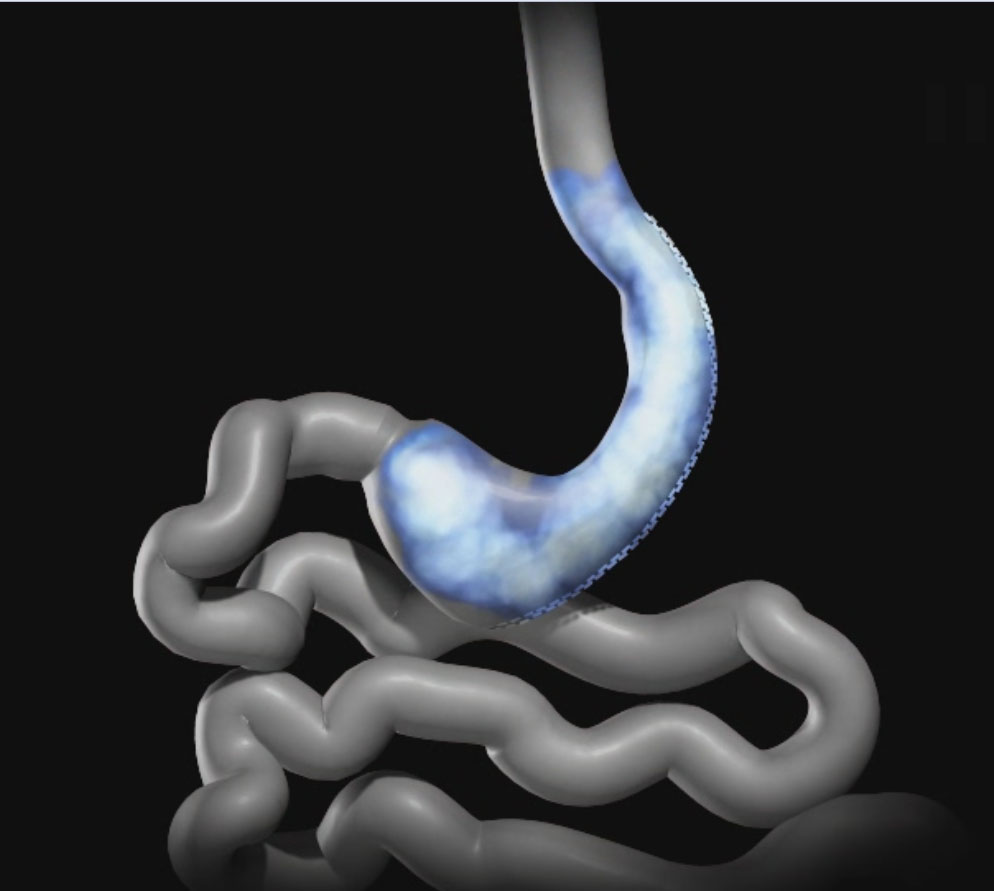
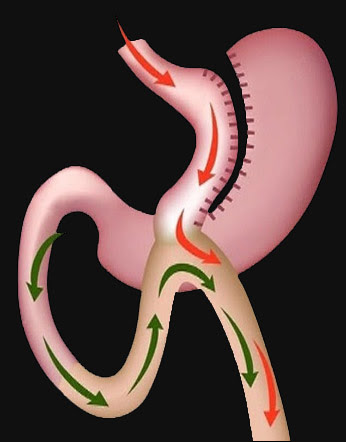
Roux-Y-Gastric Bypass (RYGB)
Laproscopic Sleeve Gastrectomy (LSG)
Mini Gastric Bypass (MGB)
Nutritional Surveillance Post Op Bariatric Surgery
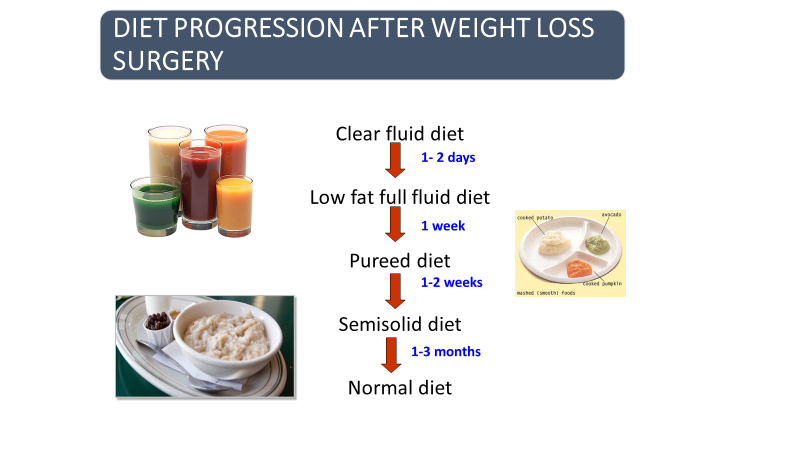
1) Within 24 hrs of surgery you are asked to start sipping water and coconut water with caution:
- i) Increase liquid volume 30-50-70-100-120-150 ml slowly.
- ii) Sip liquids do not try to finish prescribed volume at one go.
- iii) Use small cups, measuring glass or straw. Initial 24-48 hrs are assessment period to rule out your understanding about volume consumption and comfort. You need to learn new drinking and eating techniques to minimize nausea and discomfort. After 48 hrs you can have all liquids as prescribed preoperatively.
- iv) Adequate hydration after surgery is very important. You can assess your hydration status easily by urine volume and colour (not applicable in special cases like renal failure and being on some specific medicine which can change urine colour). Minimum of 1.5 to 2 litre of clear fluid consumption required at regular intervals in a day. Options are water, coconut water, clear soups, fresh unsweetened vegetable and fruit juices intake.
- v) It is important to have protein rich drinks like low-fat milk, chhachh, namkeen lassi and meal replacer every day.
- vi) If your intestine has bypassed then you need to be on a liquid diet for 3-4 weeks. Your compliance can be rewarded with some dietary modifications in week three.
- vii)If you have gone under restrictive procedures like laparoscopic sleeve gastrectomy (LSG) then your diet may be progressed to pureed after 10-15 days of surgery and followed by the semi diet.
- viii) You may resume normal eating patterns within 1-3 months, a calorierestricted normal balanced diet, aiming adequate nutrition and weight loss.
- ix) Diet advancement completely depends on your understanding, compliance with the dietary regimen and correct reporting through diet diary, 24 hrs recall or digital intake data.
- x) Be regular with follow-ups.
Nutritional Challenges after Bariatric Surgery:
“Remember, a disciplined life approach required lifelong after bariatric surgery.
……..You are on your health journey, every challenge will make you special and wiser….
Except the challenges so that you can feel the exhilaration ofvictory – George S. Patton
Nutritional challenges after bariatric surgery, more or less remain the same only degree of severity varies. Most common short-term nutritional challenges are food intolerance and altered food perceptions which include gastritis, nausea, vomiting, diarrhoea, constipation, early satiety, dumping, changes in smell and taste perception. These long persisting symptoms may lead nutritional deficiencies in the long run which may be visible as hair loss, mineral and vitamin deficiencies like iron, vitaminB12, thiamine, zinc, calcium, vitamin D and other vitamins and minerals deficiencies, weakness, pica, muscle mass loss etc. Nutritional challenges can be subdivided as mentioned below:
Gastrointestinal:
- A. Food intolerance
- Malabsorption Lifestyle associated
Gastrointestinal:
A. Food intolerance:
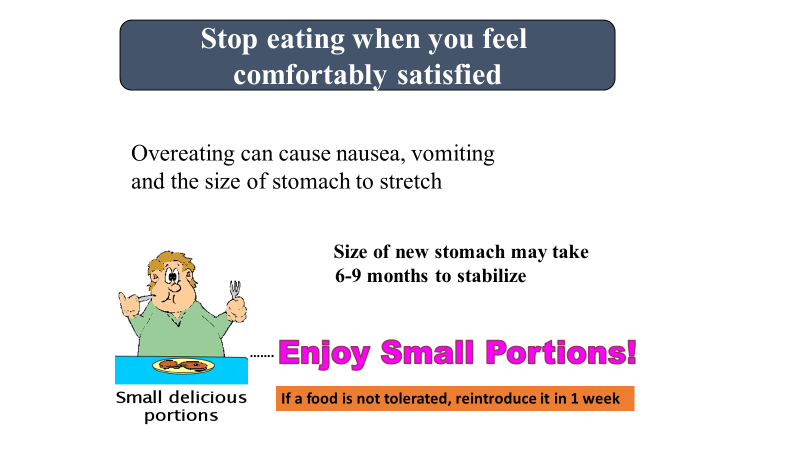
I. Nausea/vomiting: Vomiting almost always occurs during the first few months after surgery and is often described as “spitting up food that is stuck6 ” It happens usually due to overeating or not chewing food adequately. The patient should be taught that bariatric surgery has diminished the stomach’s ability to grind food into small particles. If vomiting becomes more frequent, low potassium and/or low magnesium levels often occur, requiring oral replacement. Prolonged vomiting should be considered as an indication for empiric thiamine treatment, even without, biochemical deficiency. Vomiting can signal other problems and is associated with strictures and stomal stenosis.
Practical tips for patients:
- Eat slowly- it should take a ½ hour for each meal. Chew slowly and thoroughly – at least 25 times.
- Limit fat and fatty food.
- Stop eating when you feel full.
- Introduce one new food at a time in order to rule out an intolerance. It is normal to experience intolerance to food. If a food is not tolerated, reintroduce it in 1 week.
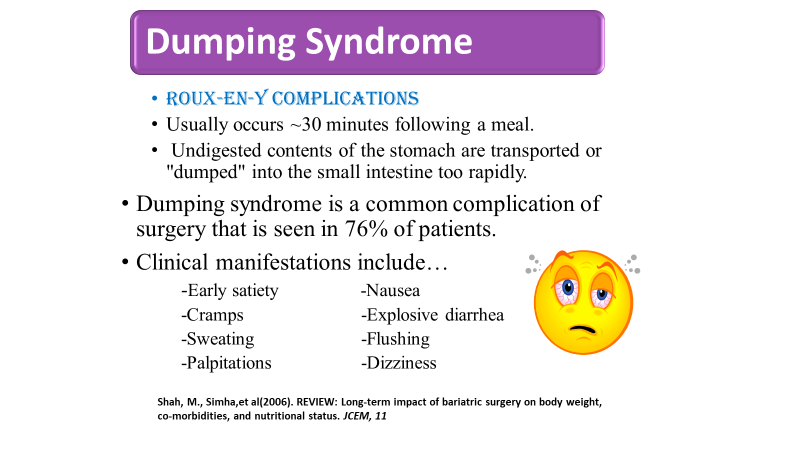
II. Dumping syndrome: “Dumping Syndrome” occurs when food passes rapidly from the stomach into the small intestine. When high osmolarity food passes rapidly through the stomach can cause an osmotic overload upon entering the small intestine. This osmotic overload brings fluid from blood vessels into the lumen of the small intestine, resulting in a vagal reaction. Dumping can be provoked by ingestion of concentrated sweets, overeating, and consuming liquids with meals. There have been reports of symptoms after the ingestion of foods high in salt and fat. The following symptoms can be seen about ½ hour after eating: nausea, faintness, lightheadedness, fullness, cramping, pain, weakness, sweating, rapid heart rate(tachycardia), and possibly diarrhoea.
Practical tips for patients:
- High sugar content food should be avoided like: cake, pastry, soft drinks, fruit juice with sugar, canned food, chocolates, desserts, cookies, jelly, ice-cream, honey, sharbat, jam etc.
- Avoid eating and drinking together.
- Stop drinking liquids 15 minutes before a meal, don’t drink with a meal, and resume one hour after a meal.
- Chew well, stop eating when you feel full.
- These symptoms usually pass within 15-20 minutes, wait till then. Take lots of water slowly to get relief.
III. Constipation: Constipation is very common problem after bariatric surgery and is more likely to occur due to inadequate fluid intake, taking iron supplements and being physically inactive. The combination of too little fluid and no food intake can work against your body’s normal routine of elimination
Practical tips for patients:
- Add fruits and vegetables (pureed for the first six weeks) at every meal.
- Whole grains and pulse should be incorporated at the appropriate time in most acceptable form to avoid intolerance and supplement dietary fiber.
- Soluble fiber can be added in the diet on a regular basis such as Metamucil, Fibercon, Benefiber Citrucel, Fiber
- Drink lots of water (1.5 to 2 lt of fluid per day).
- Inactivity can trigger a bout of constipation so exercise regularly.
- If the problem is still not resolved, the patient may advise using the laxative like Dulcolax suppository, Fleet Enema, or Milk of Magnesia. (laxatives should not be advised on a regular basis)
IV. Dehydration: Dehydration occurs frequently and is due to multiple factors. The very small surgically created gastric pouch makes it extremely difficult for patients to hold much fluid, restriction of fluid at meals and snacks, diarrhoea, long persisting vomiting or Intolerance to water. Dehydration can be very dangerous to overall health, and it can lead to constipation and poor absorption of medications and nutrients.
Practical tips for patients:
- Water consumption is the best method to prevent dehydration. If rehydration is needed, s liquids containing salt work well.
- Encourage patient to consume approximately 2 lt low/non caloric healthy drinks daily.
- The patient should be advised to drink slowly throughout the day. They should not rely on thirst as a trigger to drink.
- Caffeinated drinks should be avoided.
- Limit greasy foods, milk, and milk products in case of diarrhoea.
- Avoid very hot or very cold foods or drinks.
- Other healthy drinks such as coconut water, vegetable soup/juice, nonsweetened fruit juice, lime water etc can be advised as an option of water
- Fluids temperature can be altered for better tolerance.
- Liquids can be served in non-metallic glasses to avoid any odour.
V. Early satiety: Early satiety hinder with sufficient food consumption which badly affects total recommended protein allowances.
Practical tips for patients:
- During your meal, eat protein first, then fruits and vegetables, and then whole grains. The diet should always be high in protein and low in refined carbohydrates
- Lactose intolerance can be treated with clinically low lactose food for sufficient protein and other nutrient supplementation.

B. Malabsorption: Bariatric procedures that involve techniques to reduce gastric capacity or reroute the intestines to the gastric pouch may lead to micronutrient deficiencies. Vitamins and minerals that depend on fat absorption for optimal bioavailability, such as vitamins A, D, E, and K and zinc, won’t be fully absorbed. Food intolerance and poor eating practices can increase the chances of protein, vitamins and minerals deficiencies. Pre-existing nutritional deficiencies should be identified and treated before surgery to reduce the risk of nutritional deficiencies post operatively.
Most common nutrient deficiencies and symptoms patients experience after bariatric surgery and strategies for treatment
I. Protein Deficiency
It’s common for these patients not to feel hungry within the first six months after surgery because the hormones that regulate hunger cues have been dramatically altered. Protein is primarily absorbed in the mid ileum. This is commonly bypassed in malabsorptive bariatric procedures. This is augmented by an intolerance to protein rich food (dairy products, meat) which may lead to a net protein loss.The basic signs of protein malnutrition are hypoalbuminemia, oedema and alopecia (hair loss). A decrease in fatty/lean mass ration in certain restrictive procedures has been reported. The recommended daily intake of protein is 60 to 80 g or 1 to 1.5 g/kg of ideal body weight. Protein deficiency is less common in patients who have had gastric bypass, the sleeve, and adjustable gastric banding procedures; however, it’s a concern in those who have undergone BPD with or without duodenal switch.10 The incidence of protein malnutrition in all purely restrictive procedures is between 0-2%, gastric bypass procedures between 1-13% and in malabsorptive procedures between 13.4-18%.
Practical tips for patient
- Protein speeds wound healing, preserves lean body mass and enhances fat loss.
- To ensure patients get the protein they need, advise them to drink protein supplement, such as egg white protein powder, chicken soup, vegan protein, soy protein, flavoured whey protein concentrate or isolate powder. It’s important to ensure these are complete in high-biological protein, which should be mentioned on the label as a high PDCAAS.
- Consume low fat milk and milk products.
- Include nuts, oilseeds, pulses, a good amount of raw vegetables and sprouts to add up to your daily protein requirement.
- Maintain a diet diary for food compliance assessment.
- Follow up with Nutritionist/Dietician and report your dietary problems.
II. Iron: The pathogenesis of iron deficiency is due to the following factors: The reduced capacity of the gastro intestinal tract (GIT) to reduce dietary Fe3+ into the more absorbable Fe2+ ion due to the reduction in gastric HCL secretion. Bypassing the duodenum and proximal jejunum contribute to iron deficiency because that is the main site of iron absorption.
Iron deficiency is perhaps the most common and earliest nutritional deficiency to occur following bariatric surgery. Menstruating and pregnant females are at greatest risk. Iron deficiency can lead to anaemia and fatigue and in severe cases, can present with pica. However, it is important to emphasize that baseline iron deficiency has also been reported in up to 44% of obese adults prior to bariatric surgery which may contribute to iron deficiency postoperatively if not identified and treated. Routine multi-vitamin supplementation does not always appear to be sufficient to prevent iron deficiency after RYGB, and in most cases supplemental iron is necessary. If refractory to oral iron supplementation and correction, parenteral iron therapy or even blood transfusions may be necessary.
Practical tips for patient
- Iron – rich foods should be taken along with vitamin c rich foods
- Tea and coffee should not be taken with a meal. Keep at least an hour gap between a meal and caffeine- rich beverages.
- Iron and calcium supplementation should not be taken together if ratio of calcium and iron is as high as 3 mg of calcium to 0.01 mg of iron.
III. Calcium and Vitamin D
25 to 80% of adult pre-bariatric patients may have baseline vitamin D deficiency. Overweight and obese individuals tend to have lower mean levels of 25-OH D compared with lean subjects. Potential explanations include decreased dietary intake of fortified milk products, more sedentary lifestyle and reduced exposure to bright sunlight as well as sequestration of the fat-soluble vitamin in increased adipose tissue stores. Low serum 25- OH D appears to be inversely proportional to increasing fat mass.
Practical tips:
- In addition to high dietary calcium intake 2 gm/d an additional 1.5 gm/d calcium citrate has recommended.
- Calcium citrate is easier to absorb, particularly in conditions with reduced stomach acid, and is therefore preferable for patients after bariatric surgery. Taken three times a day, calcium citrate + vitamin D supplements can provide up to1500 –1800 mg of calcium and 1200– 1500 IU of vitamin D. While these amounts of calcium and vitamin D are likely to be sufficient for patients after the purely restrictive procedures, patients after RYGB may require additional supplemental vitamin D3.
IV. Other fat soluble vitamins:
Fat-soluble vitamin deficiencies, including vitamin A,D,E,K are less common after sleeve and RYGB and MGB surgeries but should be considered for routine investigation after any bariatric surgery procedure if symptoms develop.
1. Vitamin B12: Vitamin B12 plays an integral role in metabolism and helps manufacture red blood cells and maintain the central nervous system. vitamin B12 deficiency is defined as a level below 200 pg/ml. Stomach acid is needed to release vitamin B12 from protein foods. It’s unclear how much intrinsic factor is produced in the new pouch after gastric bypass surgery or sleeve gastrectomy. Intrinsic factor binds with B12 in the duodenum for absorption in the lower intestines. Body stores of vitamin B12 are substantial at about 2000 µg, with the average daily requirement being only 2 µg.
Low vitamin B12 levels have been reported prior to bariatric surgery in up to 18% of severely obese adults. Vitamin B12 deficiency post-operatively is more commonly associated with RYGB (up to one- third of patients), but the rate is significantly reduced to approximately 4% of patients with vitamin B12 supplementation. Multivitamin supplementation alone is not sufficient to prevent the vitamin B12 deficiency. Daily oral vitamin B12 (350 – 600 ug per day) is effective in correcting deficiency in 81 to 95% of patients and intramuscular monthly vitamin B12 injections are another option in patients who have trouble adhering to daily oral supplements.
Practical tips
- The nonvegetarian option should be included
- Low- fat milk is also a fair source of Vitamin B12
V. Folic Acid: Low prevalence of folate deficiency has been identified (0–6%) at baseline. Similarly, risk of folate deficiency appears to be very low after bariatric surgery and the addition of a routine multivitamin nearly always corrects any deficiencies. This is likely due to the absorption of folate along the entire length of the small intestine and bacterial synthesis of folate in the intestine. Low folate levels after bariatric surgery, therefore, can indicate a lack of adherence to multivitamin supplementation.
Practical tips:
- The gastric sleeve, although less invasive than the gastric bypass procedures, may result in a higher risk of folate deficiency. The study by Gehrer showed that 22% of gastric sleeve patients were low in folic acid post-surgery and normal levels were restored when patients received a daily 1-mg folic acid supplement.
- Green leafy vegetables, beans and legumes, fortified food, citrus fruits and juices are rich source of folic acid.
VI. Thiamin (B1) Deficiency:
Thiamine is absorbed throughout the duodenum, although preferentially in the more acidic environment of the proximal portion. Body stores approximately 25-30 mg of thiamine, mainly in skeletal muscle, heart, brain, liver and kidneys. In a dietary deficient state, body stores can be depleted in 2-3 weeks. Thiamine is crucial in the metabolism of carbohydrate, and the administration of oral or parenteral carbohydrate is a precipitating factor for the complications of thiamine deficiency (Wernicke’s/Korsikoff’s). Thiamine status is best assessed by determining erythrocyte transketolase activity.
Pathogenesis of thiamine deficiency:
- The decrease in acid production (resulting from a decreased gastric mucosal surface area)
- Restriction of food intake
- Frequent vomiting
- Current evidence suggests prompt administration of 50-100mg/d intravenously or intramuscularly at the onset of symptoms will halt the progression and likely lead to some resolution of the complications.
- Parenteral supplementation with thiamine (100 mg/d) should be initiated in the patient with active neurological symptoms.
- After a 7-to 14-d course, an oral preparation (10 mg/d) can be used until neurological symptoms resolve.
- Thiamine rich foods are sunflower seeds, fish, beans, whole wheat, and oats etc.
VII. Zinc:
Zinc is a mineral that helps maintain the immune system and is associated with cell division, cell growth, wound healing, and carbohydrate metabolism. A zinc deficiency also may exacerbate hair loss, which is common within the first six months after bariatric surgery. Hair loss is most commonly associated with telogen effluvium, triggered by rapid weight loss and the stress of surgery on the body. Patients who are zinc deficient may experience a metallic taste in their mouths and hair loss on the arms, legs, and groin area. Research has shown that gastric bypass patients are more likely to be at risk of zinc deficiency because of zinc absorption heavily dependent on fat absorption. However, one study found that 34% of gastric sleeve patients experienced deficiency post-surgery.
- Zinc deficiency can be reversed by zinc supplementation
- Zinc- rich foods are: beans, oil seeds, nuts, non-vegetarian sources
VIII. Magnesium and selenium
These are rare deficiencies. None of these has significant clinical consequences. Heart failure following bariatric surgery should be screened carefully to rule out nutrient-deficient cardiomyopathy.
IX. Copper:
Copper is another important mineral that hasn’t been studied extensively in bariatric surgery patients despite the fact it’s absorbed by the stomach and proximal gut. This has particularly important ramifications for patients who had gastric bypass. A copper deficiency can cause anemia and myelopathy, decreased myelin in the spinal cord that may diminish function of the upper or lower extremities, similar to symptoms associated with a vitamin B12 deficiency. Copper status needs to be examined in gastric bypass patients presenting with signs and symptoms of neuropathy with normal vitamin B12 levels.
- Symptoms of copper deficiency include paresthesia’s and ataxia. Since zinc supplementation may decrease copper stores and/or exacerbate copper deficiency, patients should be aware of zinc hair or nail supplements without copper, especially long-term use of high-dose zinc supplements.
- Treatment is a multivitamin containing 2 to 4 mg/day of elemental copper, depending on the patient’s deficiency level.
Life style associated: The vast majority of weight loss after bariatric surgery is accomplished at or around 1 year after surgery. Some patients continue to lose a small amount of weight while others begin to maintain their lower weight in 12 to 18 months after surgery. At 18 to 24 months after surgery, almost all patients stop losing weight and most patients either maintain or regain weight. During the first six to 12 months after surgery, patients generally consume 900 to 1000 calories. Calorie consumption slowly increases due to a change in the pouch size and stoma size, gastric emptying rate and intake of solid food. Flanagan observed a stabilization in pouch size at two years with the average size holding six ounces
Practical tips for patients:
- Regular follow up with Dietician.
- Increase physical activity.
- Include more options for low-calorie food and non-caloric liquids to curb their hunger.
- Conducting support group meetings.
- The patient should be advised for low calorie, sufficient protein and high fibre diet.
- Compliance should be assessed periodically by diet diary, activity log book, list of grocery items in the previous month, questionnaire, interview method etc.
Other Challenges:
a. Hair Loss: Temporary hair loss can occur from rapid weight loss, but may also be caused by inadequate protein in the diet. This situation is usually temporary and responds to protein supplements.
b. Gall stone disease: very low-calorie diet rapid weight loss more than three pounds or app. 1.5 kg per week may have a 10- to 25-percent chances of developing gallstones. Most of these are “silent” gallstones, meaning that the patient doesn’t have any symptoms. Those who have normal gall bladder emptying and a small stone may respond with oral dilution therapies. Most doctors prefer ursodeoxycholic acid one of the safest common drug. Some of them need surgery.
Practical tips for patients:
- Eat a moderate amount of healthy fat as part of your diet. Munch healthy snacks like nuts, salads, roasted makhana without oil, roasted channa, in limited quantities. Do remember, nothing is calorie free except water and lime water without sugar. Eat on scheduled time. Visit more frequently with your nutritionists.
Include all forms of exercises
Support group meetings are a platform for you to share your apprehensions, weight loss success story and learn from another bariatric surgery fellow. YOU NEED TO LEARN AND UNLEARN MANY things related to lifestyle modification IN A SHORT SPAN OF TIME. SUPPORT GROUP MEETINGS HELP YOU IN YOUR PROGRESS.
RICHA JAISWAL
Registered dietician
